Keratoconus treatment in Iran is considered an advanced medical service, as cities such as Shiraz, Tehran, Mashhad, Yazd, and Ahvaz provide a wide range of advanced treatment options. Patients benefit from modern technologies and specialized medical expertise that contribute to improving the quality of life and providing effective solutions to this difficult condition. These cities are characterized by providing a therapeutic environment that supports patients during their treatment journey, making Iran a preferred destination for those seeking innovative and safe treatments for keratoconus.
The content of this article is only to increase your awareness. Before taking any action, consult our doctors for treatment
Table of contents
- Introduction.
- What is keratoconus?
- How does keratoconus occur?
- What are the early symptoms and complications of keratoconus?
- How is keratoconus diagnosed?
- Treatment of keratoconus.
- Reference
1. Introduction
Keratoconus is an eye disease that affects the structure of the cornea and causes vision loss and even blindness in severe cases. This disease usually begins in puberty and develops until the middle of the third decade of life, that is, between thirty and forty years.
About one in 2,000 people develop keratoconus. The early stages of this disease can be treated with glasses, but as the disease progresses into late childhood or early adulthood, a corneal transplant may be needed for treatment.
Stay with us so we can examine the symptoms, complications, and treatment of keratoconus.
You should see an ophthalmologist to diagnose and treat keratoconus. You can get to know our best eye specialists in Iran in Shiraz, consult them online or by phone, and if necessary, schedule a personal visit.
2. What is keratoconus?

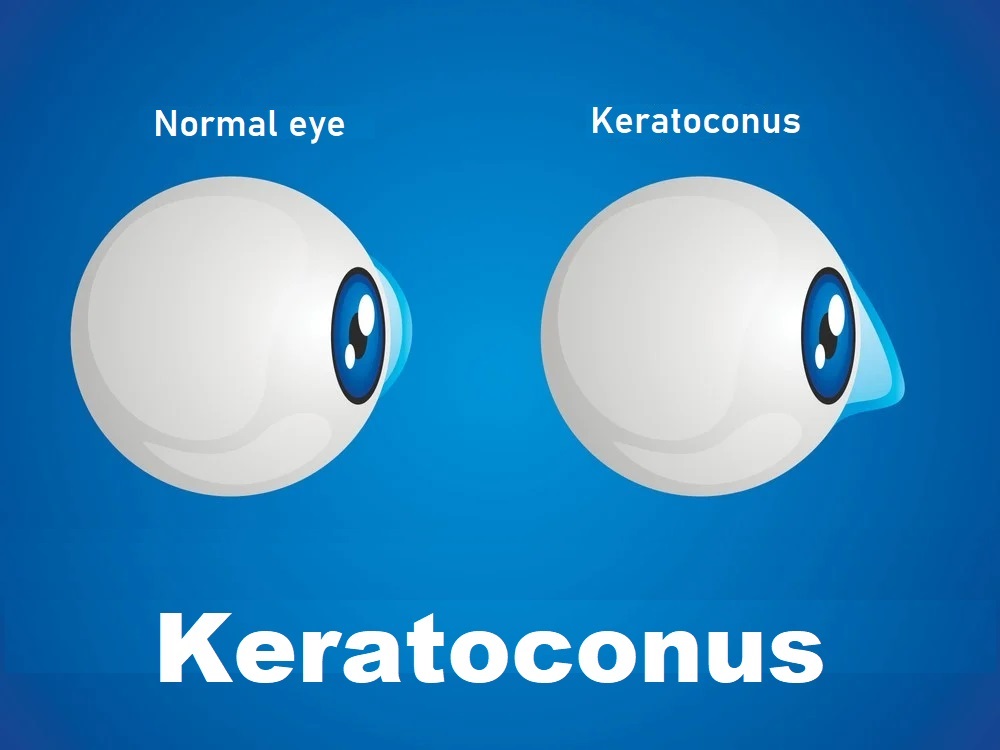
Keratoconus is characterized by thinning of the cornea and irregularities in the corneal surface. The cornea is the colored outer layer of your eye. The middle layer is the thickest part of the cornea, which is made up mostly of water and a protein called collagen. Collagen makes the cornea strong and elastic and helps maintain its regular, round shape. In fact, the cornea’s job is to focus light so you can see clearly. Keratoconus causes a person’s cornea to thin and become irregular and convex. As a result, light does not focus well on the retina and you may not see surrounding images well.
As we mentioned, this disease usually begins at puberty and develops until the middle of the third decade of life. There is no way to predict how quickly this disease will develop. Keratoconus usually affects both eyes and is more severe in one eye and affects it more.
3. How does keratoconus occur?
Despite years of research, the exact cause of keratoconus remains unknown. It is believed that the main cause of this disease is genetics. This means that some people are born with a predisposition to this disease. Since keratoconus is caused by the destruction of collagen in the cornea, an imbalance between the production and destruction of corneal tissue may be another cause of this disease. In general, the following factors can cause keratoconus.
- Genetics:
Patients who have a family history of keratoconus or have certain systemic disorders and chromosomal abnormalities such as Down syndrome are more likely to develop this disease. - Chronic eye inflammation:
Continuous inflammation resulting from exposure to stimuli and allergies contributes to the destruction of corneal tissue. As a result, these problems may cause keratoconus. - Eye scrub:
Rubbing the eye repeatedly over time damages the cornea and may lead to keratoconus. Also, if you already suffer from this disease, rubbing your eyes will speed up the progression of keratoconus. - The age:
Keratoconus usually occurs in adolescence, but may appear early in childhood. Of course, it goes without saying that people over the age of forty can also develop this disease, but the probability is very low. - Human races and races:
A study of more than 16,000 patients with keratoconus showed that people of black or Hispanic descent are approximately 50% more likely to develop this disease than other races. - Other eye diseases:
Atopic eye disease is a disease that causes the breakdown of corneal tissue and may cause you to develop keratoconus. Retinitis pigmentosa is another disease that affects the cornea. In general, many eye diseases can cause keratoconus. So, if you suffer from an eye disease, it is best to consult your doctor about the possibility of keratoconus.
4. What are the early symptoms of keratoconus?

Many keratoconus patients are not aware of this disease. The first symptom is mild blurred vision that gradually becomes more severe and does not correct. Other symptoms of keratoconus include:
- See normal lights as glare or notice a halo around the lights when you look at them.
- Poor night vision.
- Burning sensation in the eye or headache with eye pain.
- Increased sensitivity to bright light.
- Vision suddenly blurs.
- Myopia (difficulty seeing distant objects).
- Irregular astigmatism.
- Constant desire to rub eyes.
- Eye fatigue.
- In rare cases, the cornea may ulcerate, causing ulcers and swelling in the eye.
- In some cases, keratoconus may swell quickly, causing sudden loss of vision and scarring of the cornea. This is caused by a breakage of the inner lining of the cornea and the fluid surrounding it (edema) enters. This swelling usually goes away on its own, but it may cause scarring in your eye that affects your vision.
- In advanced cases, keratoconus may cause scarring in the conical portion of the cornea, which may cause blindness.
5. How is keratoconus diagnosed?


To diagnose keratoconus, your ophthalmologist will review your medical and family history and perform an eye examination. Also, to accurately diagnose this disease, it is necessary to perform more detailed tests on your eyes. The following tests are examples of such tests:
- Eye refraction
This test uses special equipment to measure eye characteristics. You may be asked to look through a device equipped with wheels with different lenses, called a vision motor. This device helps determine which combination of objects gives you the clearest view. Some doctors may use a portable device – called a retinoscope – to evaluate the eyes. - Slit lamp examination
This test involves shining a vertical beam of light onto the surface of the eye and examining it using a low-power microscope. The ophthalmologist evaluates the shape of the cornea and looks for other possible problems in the eye. - Keratometry
This examination involves focusing a circle of light on the cornea and measuring the reflectivity. This determines the basic shape of the cornea. - Computerized corneal planning
Special imaging tests, such as tomography of the cornea and tomography of the cornea, take pictures to draw a detailed map of the shape of the cornea. A corneal CT scan can also measure the thickness of the cornea. This type of test can often detect early signs of keratoconus before it can be seen on a slit-lamp examination
6. Methods of treating keratoconus in Iran, Shiraz
- Use of glasses:
If the disease is in its early stages, prescribing glasses can help the eye recover. But it should also be noted that the degree of glasses will also change as vision changes. - Wearing contact lenses:
If the disease progresses and is not corrected by a prescription for vision glasses, the doctor will prescribe rigid contact lenses. - Use of UV light or cross-linking (Collagen Cross-Linking, CXL, C3R, or CCL):
In this method, the collagen fibers in the cornea are linked by ultraviolet rays and with the help of riboflavin, which makes the cornea stronger. - Use of intracorneal rings:
One method of treating keratoconus is the use of intracorneal rings, which are used in some cases of mild to moderate keratoconus that cannot tolerate contact lenses. These rings reduce irregular astigmatism in the eye and correct vision. - Corneal transplant:
If keratoconus has progressed significantly, contact lenses and intracorneal rings will not help, and a corneal transplant should be performed.
Reference:
Kandel H, Pesudovs K, Watson SL (March 2020). “Measurement of Quality of Life in Keratoconus”. Cornea. 39 (3): 386–393.
Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS (1 August 2010). “Keratoconus: a review”. Contact Lens & Anterior Eye: The Journal of the British Contact Lens Association. 33 (4): 157–166, quiz 205.
Jamali H, Heydari M, Masihpour N, Khosravi A, Zare M, Shams M, Omrani GR (2023). “Serum androgens and prolactin levels in patients with keratoconus”. Clin Exp Optom. 106 (5): 484–488
Harthan JS, Gelles JD, Block SS, Tullo W, Morgenstern AS, Su B, Chung D, Yu A, Greenstein SA, Hersh PS, Eiden SB (1 March 2024). “Prevalence of Keratoconus Based on Scheimpflug Corneal Tomography Metrics in a Pediatric Population From a Chicago-Based School Age Vision Clinic”. Eye & Contact Lens. 50 (3): 121–125
Read more about other articles in the medical fields (Cosmetics and Medical).
- Hair Transplantation in Iran
- Rhinoplasty (Nose Job in Iran)
- Face Lift Surgery (Rhytidectomy) in Iran
- Breast Lift in Iran
- Chin Surgery in Iran
- Liposuction in Iran
- Tummy Tuck (Abdominoplasty) in Iran
- Butt Augmentation (Brazilian butt lift)
- Breast Augmentation in Iran
- Eye Care in Iran
- Cataract Surgery in Iran
- Diabetic Retinopathy Treatment in Iran
- Heart Surgery in Iran
- Knee Replacement in Iran
- Eyelid Surgery in Iran
- Safe Abortion in Iran
- Fertility Treatment in Iran


